Médecins Sans Frontières/Doctors Without Borders (MSF) is particularly concerned about five diseases that have the potential to become epidemics since 2016.
Without proper investment in preventing and responding to outbreaks of cholera, malaria, measles, meningitis and a group of often-overlooked diseases spread by viruses and parasites, they are likely to pose an ever greater threat to people’s health in the year ahead.
Current strategies to prevent major outbreaks of disease show only limited success.
Emerging and re-emerging diseases
Epidemics continue to occur, often with devastating consequences for some less developed countries by opening cracks in national health systems and exhausting available resources.
“We know that thousands of lives will be at risk in the year to come, although the means exist to prevent these deaths,” says Dr Monica Rull, operational health advisor for MSF.
“Epidemics of cholera, malaria, measles and meningitis take place every year, with these diseases incapacitating and killing many – and this needs to stop.
“At the same time, the threat posed by emerging and re-emerging virus and parasite-spread diseases – such as dengue fever, Zika, Ebola and Kala Azar – needs to be faced.”
Five epidemics to watch:
Cholera
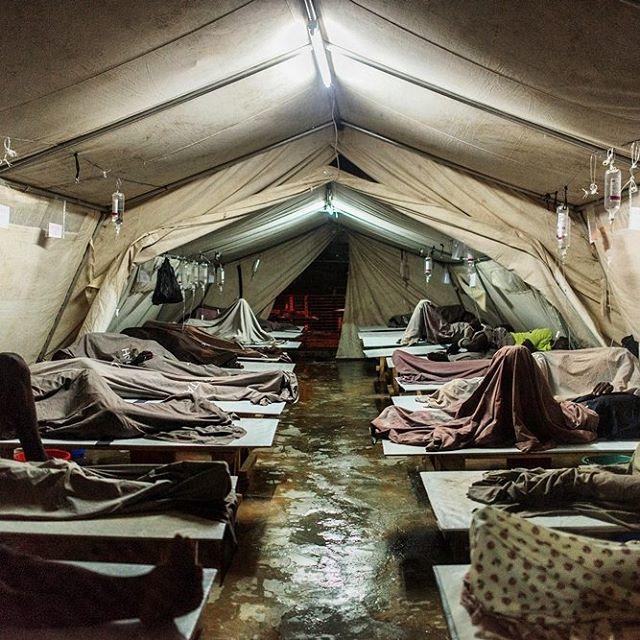
Cholera is a water-borne, gastrointestinal infection that causes acute watery diarrhoea and vomiting, which can lead to severe dehydration and death within hours if left untreated.
In 2014, we treated 46,900 people for cholera in 16 outbreaks affecting six countries (Cameroon, Democratic Republic of Congo (DRC), Haiti, Niger, Nigeria and South Sudan).
MSF asks:
- There are only two WHO pre-qualified vaccines available. The most adapted vaccine for outbreak response is produced by an Indian company that has no capacity to scale-up production to cover worldwide needs. The majority of doses are available only through the stockpile system. There is a need to scale-up production and for more options to be validated by the WHO.
- Currently a two dose strategy is recommended. According to researchers, a single dose strategy may prevent more cases than a two dose strategy that is given to half as many people. More flexibility on the allocation of vaccines and support from the WHO for single dose campaigns is required.
Find out more about our work with cholera
Malaria

Malaria is transmitted by infected mosquitoes. Severe malaria can lead to organ damage and death if left untreated.
In 2014, we provided treatment to 2,114,900 patients affected by malaria, and gave seasonal malaria chemoprevention (SMC) to more than 750,000 children below five years of age.
MSF asks:
- Increase the availability of injectable artesunate for the treatment of severe malaria, and increase blood transfusion capacity,
- Adapt the vector control tools according to emerging trends of resistance to insecticides,
- Reinforce malaria surveillance and define the outbreak threshold per country, per region and per district to improve alert mechanisms.
- The WHO should provide better guidance for the use of preventative strategies, such as seasonal malaria chemoprevention, mass drug administration, intermittent preventive treatment and focused screening and treatment for outbreaks,
- Free malaria treatment during outbreaks or seasonal peaks needs to be guaranteed.
Find out more about our response to malaria outbreaks
Measles

Measles is a highly contagious viral disease, for which there is no specific treatment. In high-income countries, most people infected with measles recover within two to three weeks, and mortality rates are low.
In developing countries, however, the mortality rate can be three to 15 percent, rising to 20 percent during outbreaks and in areas where people are more vulnerable.
In 2014, we treated 33,700 patients for measles and vaccinated 1,513,700 people in response to outbreaks.
MSF asks:
- Patients should be treated for free during a measles outbreak (including for associated pathologies, such as malaria).
- There is a need for greater involvement of emergency actors and the Ministry of Health in the provision of case management.
- Long-term vaccination campaigns should support, not block, epidemic response
- Need better surveillance and early declaration of outbreaks – flexibility and reactiveness.
- The response needs to be adapted to each outbreak, as the one solution/strategy for all is not working.
Find out more about MSF's work responding to measles
Meningitis

Meningitis is the inflammation of the thin membranes surrounding the brain and the spinal cord. It is most often caused by infection – bacterial, viral or fungal.
Meningitis occurs throughout the world, but the majority of infections and deaths are in Africa, particularly across the ‘meningitis belt’, an east–west geographical strip than runs from Ethiopia to Senegal.
In 2014, we vaccinated 75,100 people against meningitis in response to outbreaks.
MSF asks:
- Rational use for highest impact – focus on the medical and outbreak control criteria,
- Encourage diversification of manufacturing and procurement channels to ensure a rapid response when an outbreak occurs,
- Manufacturers need to ensure that – at the very least – their commitment to the ICG is fulfilled and they should increase vaccination production immediately,
- The WHO need to push/accept/promote alternative strategies to vaccination to protect individuals and limit outbreaks (e.g. mass distribution of antibiotics).
Find out more about MSF's work responding to meningitis
Neglected diseases

Outbreaks of dengue, Chikungunya, Zika, Middle East Respiratory Syndrome (MERS) and haemorrhagic fevers have all been reported in 2015. Parasitic infections such as visceral leishmaniasis (kala azar) that were under control are now on the rise again.
In 2014, we treated 4,700 Ebola confirmed patients, 1,700 patients for Chikungunya and 9,500 patients for kala azar including responding to an outbreak affecting South Sudan.
MSF asks:
- Identify and declare outbreaks in order to speed up vector control measures,
- Capacity building and training for better identification of diseases, case management and infection control,
- Step up health education to avoid risky behaviour, and inform the affected population about the diseases and what to do if infected,
- Research and development for diagnostics, vaccines and treatments.
Find out more about our work with neglected diseases, like kala azar
Research and development
Along with prevention measures, resources must be provided to build effective emergency response systems. This must be part of a broader effort to help countries strengthen their health infrastructure and capabilities and provide health education to local communities.
Rapid alert mechanisms must be accompanied by rapid response activities once a disease breaks out, with free and quality medical care provided to all those affected.
The research and development agenda must be reoriented towards the greater public good, with a recognition that market forces cannot be counted on to deliver effective, accessible and affordable tools for under-served population groups.
MSF emphasises that the first step to global health security is individual health security, including for the sickest and most vulnerable people.
“Current outbreak response strategies are failing the very people they are designed to help,” says Dr Rull. “If we don’t make significant changes, we will be doomed to repeat past mistakes, and must take responsibility for the consequences.”





