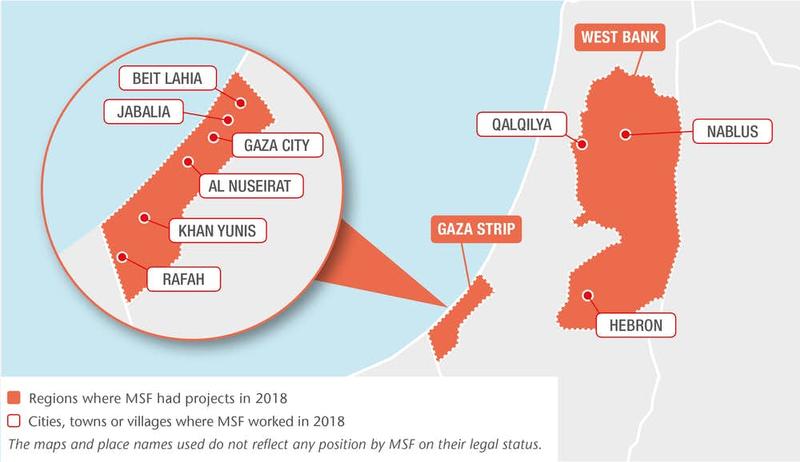
In 2018, Médecins Sans Frontières (MSF) provided specialist surgical and post-operative care to huge numbers of patients with complex gunshot injuries in Gaza, and responded to growing mental health needs in the West Bank.
[[Country-Facts]]
Gaza’s fragile health system was overwhelmed by the number of people returning from protests with complex gunshot wounds throughout much of 2018.
We drastically scaled up our operations in response to the needs of these severely injured patients, while continuing to run clinics for burns patients in the blockaded enclave and provide mental healthcare in the West Bank.

Gaza
According to the World Health Organization, 6,239 people were injured by Israeli army bullets during protests along the fence that separates Gaza from Israel between 30 March and 31 December.
Nearly 90 per cent of these injuries were to lower limbs. Half were open fractures, often with serious damage to the bone; many of the others involved severe tissue loss and extensive damage to the nerves and vascular system.
These are complex and severe injuries that require long and careful follow-up. While MSF and other medical organisations provided initial lifesaving surgery for some of the wounded, the Ministry of Health provided the first line of response in most cases, stopping the bleeding and fitting external fixators for patients with more severe or complex fractures.
After being discharged, many were admitted to our care for further surgery to clean and close large, open wounds and perform regular dressing changes.
Bone infection is a risk for many of the patients with open fractures: experience from MSF projects in other Middle Eastern conflict areas suggests that between 25 and 40 per cent may be affected.
The lack of laboratory capacity in Gaza means it is not possible to adequately test for infections in most patients. And yet it is only once a wound is stabilised and free of infection that the process of rebuilding the bone can begin.
Afterwards, these patients will continue to require long periods of care and physiotherapy to return function to badly damaged limbs.
By the end of the year, we were running five clinics, offering wound dressings, physiotherapy and pain management. We also increased our surgical capacity, opening an inpatient department for our surgical patients in Al Awda hospital in Jabalia, and performing plastic and orthopaedic surgery in Al Shifa and Dar Al Salam hospitals.
We made a number of emergency surgical interventions in other hospitals and clinics throughout the year to address the growing demand for care for the wounded. We ran a surgical programme in Yousef al-Najjar hospital from July to December and sent vascular surgeons to Al Aqsa hospital between April and June.
By 31 December, we had received over 8,000 patients in our post-operative clinics, including 3,780 trauma patients. Our teams changed 107,140 dressings, conducted almost 66,000 physiotherapy sessions and operated on over 1,500 trauma patients, performing 2,320 surgical interventions.
In December, we were still following up 900 trauma patients.
Despite the huge increase in our activities, the Gazan health system, already crippled by over 10 years of blockade, remains unable to cope with the large number of patients with complex injuries.
It is therefore possible that a lack of capacity for reconstructive surgery, and the inability to prevent and treat bone infections, will lead to a wave of delayed amputations.
In addition to our work with trauma patients, we admitted 4,475 burns patients to our post-operative clinics in 2018, carrying out surgical procedures on 129 of them. The number of admissions was stable compared with 2017 but more than twice as many as in 2015.
The West Bank
We continue to run mental healthcare programmes in the West Bank, where the ongoing occupation, violence and socioeconomic insecurity have taken a severe toll on residents.
In 2018, we refocused our mental health support for victims of political violence in Hebron around a strategy of increased engagement with the community in the form of outreach activities. This support was delivered against a backdrop of increasing violence by Israeli settlers towards Palestinians.
Hebron is one of the locations in which attacks most frequently occur, and most of our patients there had been directly or indirectly exposed to violence: their house may have been raided by the armed forces, or a family member detained, arrested, injured or killed. They suffered from anxiety, depression and adjustment disorders as a result.
In 2018, our teams in Hebron offered psychotherapy, individual and family counselling, mental health awareness sessions and psychoeducational support. More than 1,400 people received psychological first aid, 370 benefited from psychotherapy or counselling, and 8,800 attended group activities over the year.
We also provide mental healthcare for people with various moderate to severe mental health issues in the cities and villages of Nablus and Qalqilya governorates. The main illness we see here is moderate to severe depression, which accounts for 40 per cent of cases and can in many cases be attributed to the occupation and the tensions and violence it creates.
However, in 2018 our teams received an increasing number of cases of dysfunctional family and domestic violence, which also have a serious impact on mental health. We ran a total of 2,520 psychotherapy sessions in Nablus and Qalqilya throughout the year and admitted 284 new patients for care; 40 per cent of our patients were under 18 years old.
Find out more in our 2018 International Activity Report



